Table of Contents
ToggleCancer of the cervix is highly preventable and treatable if diagnosed early, yet it is the most common and fatal cancer among women. This cancer is a major cause of morbidity and mortality. The reason behind this is that several women are still unaware of its causes and symptoms. Tech Mahindra Foundation SMART Healthcare Academies undertook an initiative to create awareness about cervical cancer and ways to prevent it. The स्मार्ट हेल्थकेयर अकादमी organised a webinar, and as a speaker, I was delighted to be a part of the awareness efforts. I disseminated information about the causes, symptoms, treatment and prevention of cancer of the cervix. This blog will help paramedics and women learn:
- What are the risk factors?
- What are the symptoms women should look for?
- What are the different screenings?
- How can women minimize their risk level?
So, let’s learn more about cervical cancer so you can reduce the risk of cancer, by maintaining a healthy lifestyle and performing regular screenings.
What is Cervical Cancer?
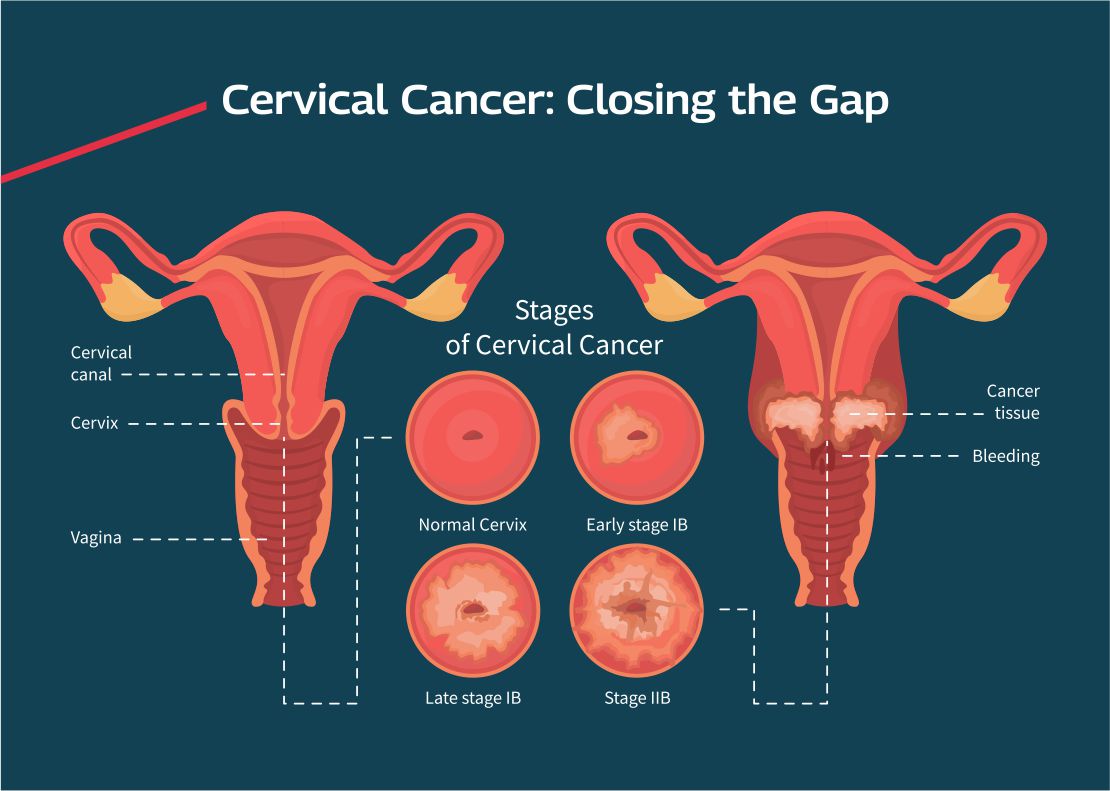
Cervix cancer is the fourth most common cancer among females across the globe. Cervical cancer is the uncontrolled growth of abnormal cells in the cervix lining. It is preventable and successfully treatable if diagnosed early and managed effectively. Screening, treatment of pre-cancer lesions and HPV vaccination are the most cost-effective ways to prevent cervical cancer.
What are the Causes of Cervical Cancer?
The most significant risk factor for cervix cancer is an infection with a high-risk strain of the human papillomavirus (HPV). HPV infections are sexually transmitted infections. Not all HPV infections lead to cervical cancer, however, HPV 16 and 18 are the most common high-risk strains that cause cervical cancer. The other causes of cervical cancer include:
- A high number of pregnancies
- Multiple sexual partners
- Early sexual activity
- Smoking
- Weakened immune system
- Other sexually transmitted infections like chlamydia, syphilis, HIV/AIDS, and herpes.
- Irrespective of age, all females risk exposure to the HPV virus as it can spread via skin contact and sexual intercourse.
What are the Symptoms of Cervix Cancer?
A cervical screening test is the only way to check if there are abnormal cells in your cervix that may develop into cancer. The symptoms of cervix cancer in its early stages are rare and are only seen in the advanced stages. The most common symptoms of this cancer are as follows:
- Bleeding after intercourse
- Pain during intercourse.
- Abnormal vaginal discharge that is not responding to the treatment.
- Post-menopausal bleeding
- Bleeding between periods
- Pelvic pain or a low backache
- Unexplained loss of weight
- Anaemia
- Menstrual bleeding that is either longer or heavier
What is the Treatment for Cervix Cancer?
Recommended cervical cancer treatment depends on various factors, including the cancer stage, size of the tumour, age, desire to have children, and general health. The treatments for cancer of the cervix are surgery, radiation, chemotherapy, targeted therapy, and immunotherapy.
- Surgery
Often surgery is the main treatment. If diagnosed at an early stage, the doctor may remove the area of the cervix that contains cancer cells. When the cancer is invasive, a hysterectomy or trachelectomy is used to treat it. In other words, when the cancer is widespread, the surgery involves removing the cervix, ovaries, fallopian tubes, uterus, and other organs in the pelvis. Along with the surgery, you may need radiation and chemotherapy.
- Radiation
In this treatment, high-energy X-ray beams are used to kill cancer cells and stop their growth. Radiation affects cancer cells only in the area that is treated. Radiotherapy can be external, internal, or both.
- Chemotherapy
Drugs are given to kill cancer cells throughout the body. Chemotherapy is done in cycles of intensive treatment followed by recovery periods.
How Can You Prevent Cervix Cancer?
This cancer is highly preventable and curable if detected early. Spreading awareness about cancer, its symptoms, HPV vaccination, routine screening, and follow-up treatment can help prevent nearly all cervical cancers. Besides these measures routine screening, vaccination and quitting smoking can help prevent cervical cancer.
- Routine Screening
Regular screening with colposcopy, liquid-based cytology, HPV and Pap tests helps prevent cervical cancer. The tests can detect abnormal cell changes and precancerous conditions of the cervix that can be treated before they turn into cancer. People with a cervix should start a regular screening in their early 20s.
1. Colposcopy:
It is a technique of observing the cervix under magnification. It facilitates various tests which will outline the lesions on the cervix. Colposcopy should be done once every five years.
How to Prepare Yourself for a Colposcopy?
Before a Colposcopy
-
-
- You should not be in your periods (No Periods)
- No intercourse one day before
- No douching or vaginal creams
- Shave your private parts
-
After The Colposcopy
-
-
- No rest required
- Take panty liner
- Avoid intercourse for three days
- Results within five days
- Follow-up with a doctor regarding further treatment
-
2. Liquid-Based Cytology (LBC):
It is a new technique for collecting cytological samples to detect cervix cancer.
3. HPV Tests:
It checks for the genetic material (DNA) of the human papillomavirus. The human papillomavirus has high oncogenic potential. The sample collection is similar to the Pap smear test.
- HPV Vaccination An HPV vaccination may reduce the risk of cervical cancer and other HPV-related cancers. Since HPV is a sexually transmitted infection, having safe sex reduces your risk of cervical cancer. Further, taking measures such as limiting the sexual partners and using a condom every time will also help prevent sexually transmitted infections.
What are the Different Types of HPV Vaccination?
There are three types of HPV vaccinations available to prevent cervical cancer. The bivalent vaccine protects against HPV 16 and HPV 18 strains. The quadrivalent vaccine offers protection against four types of HPV strains (6, 11, 16 and 28). The non-valent form of the HPV vaccine protects against nine HPV strains (6, 11, 16, 28, 31, 33, 45, 52, and 58). However, all three vaccines protect against HPV 16 and 18 strains that cause most HPV cancers.
How Does the Vaccine Work?
The vaccine gets your body to produce antibodies against the HPV virus. These antibodies protect your body from an HPV infection by fighting the virus when it tries to attack the cervix.
Who Should Take the Vaccine and When?
Ideally, the vaccine should be taken as early as possible after the age of 9 years, but females of any age, up to 45 years, can benefit from this vaccine. Expectant mothers should not take the vaccine during their pregnancy.
What is the Dosage of the HPV Vaccine?
The first dose is administered at an elected date. The second dose is given after two months of the first dose, and the third dose is given after six months of the first dose.
- Don’t Smoke: Women who smoke are at an eight times higher risk of developing cervical cancer. So, if you smoke or use tobacco products, talk to your doctor or general practitioner about ways to quit smoking.
Final Words
There is no definite way of cancer prevention, but regular screening can help in early cancer detection and increases your chances of survival and successful treatment. You must consult your doctor if you see any changes or abnormalities or have pain. Routine screening, along with HPV vaccination, provides effective protection against cervical cancer. You can easily get yourself vaccinated at your doctor’s clinic or a hospital.

